sprout at a glance
On September 20, 2022, Ugandan health authorities declared an outbreak of Ebola disease, caused by the Sudan virus, following laboratory confirmation of a patient from a village in Madudu sub-county, Mubende district, Uganda. central.
As of September 25, 2022, a cumulative number of 18 confirmed cases and 18 probable cases have been reported in Mubende, Kyegegwa and Kassanda districts, including 23 deaths, of which five were among confirmed cases (CFR among confirmed cases 28%). This is the first outbreak of Ebola caused by the Sudan virus (SUDV) in Uganda since 2012.
Description of the outbreak
On September 20, 2022, Ugandan health authorities declared an outbreak of Ebola disease caused by the Sudan virus (SUDV), after a case was confirmed in a village in Madudu sub-county in Mubende district, Central Uganda.
The case was a 24-year-old man who developed a wide range of symptoms on 9/11, including high fever, tonic seizures, vomiting blood and diarrhea, loss of appetite, pain on swallowing, chest pain, dry cough, and bleeding. In the eyes. He visited two private clinics successively between 11-13 and 13-15 September with no improvement. He was subsequently referred to the Regional Reference Hospital (RRH) on September 15, where he was isolated as a suspected case of viral hemorrhagic fever. A blood sample was collected on September 17 and sent to the Uganda Virus Research Institute (UVRI) in Kampala, where RT-PCR tests performed were positive for SUDV on September 19. On the same day, the patient died.
Preliminary investigation results identified a number of community deaths from an unknown disease in Madudu and Kiruma sub-counties of Mubende district reported in the first two weeks of September. These deaths are now considered probable Ebola cases caused by SUDV.
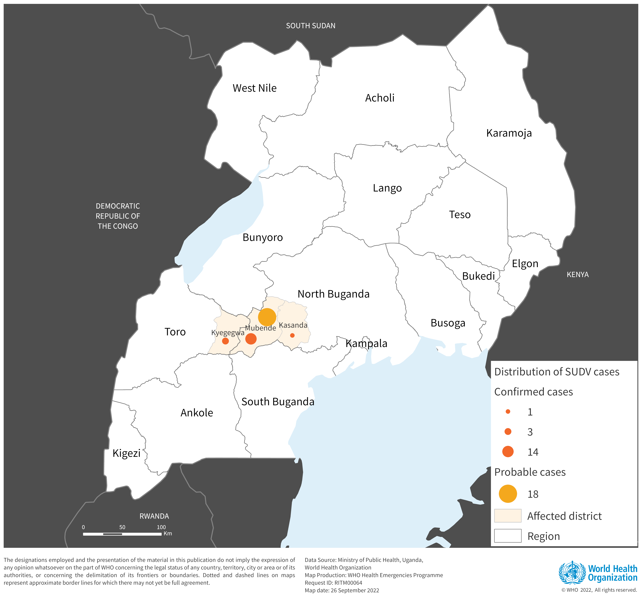
As of September 25, 2022, a cumulative number of 36 cases (18 confirmed and 18 probable) have been reported in Mubende (14 confirmed and 18 probable), Kyegegwa (3 confirmed cases), and Kassanda (1 confirmed case) districts. There have been 23 deaths, of which five were among confirmed cases (CFR among confirmed cases 28%). Of the total confirmed and suspected cases, 62% are women and 38% are men. There are currently 13 confirmed cases hospitalized. The median age of the cases is 26 years (range 1 year to 60 years). A cumulative number of 223 contacts have been listed.
Map of confirmed (n=18) and suspected (n=18) cases of Ebola virus disease from Sudan, by district, Uganda (as of 25 September 2022).
disease epidemiology
According to the International Classification of Diseases for Filoviruses (ICD-11) published in May 2019, Ebola is now subcategorized based on the causative virus. Outbreaks of Ebola disease caused by the Sudan virus are called Sudan virus disease (SVD) outbreaks. Before May 2019, all the viruses that caused Ebola were grouped together. Based on the results of laboratory tests, this outbreak is caused by the Sudan virus.
Sudan virus disease is a serious, often fatal disease that affects humans. Sudan virus was first reported in southern Sudan in June 1976, since then the virus has emerged periodically and seven outbreaks caused by SUDV have been reported so far, four in Uganda and three in Sudan. Estimated SVD case fatality rates have ranged from 41% to 100% in previous outbreaks.
The virus is introduced into the human population through close contact with the blood, secretions, organs, or other body fluids of infected animals such as fruit bats, chimpanzees, gorillas, monkeys, forest antelope, or porcupines that are sick, dead, or in the tropical rainforest. The virus then spreads through person-to-person transmission through direct contact (via broken skin or mucous membranes) with the blood or body fluids of a person who is sick or has died from it. of SVD or objects that have been contaminated with body fluids (such as blood, feces, vomit) from a person sick with SVD or the body of a person who died of SVD.
The incubation period varies from 2 to 21 days. People infected with the Sudan virus cannot spread the disease until they develop symptoms and remain infectious as long as their blood contains the virus. Symptoms of SVD can be sudden and include fever, fatigue, muscle pain, headache, and sore throat, followed later by vomiting, diarrhoea, rash, symptoms of impaired kidney and liver function. In some cases, the patient may experience both internal and external bleeding (for example, bleeding gums or blood in the stool).
Diagnosis of SVD can be difficult, as the early nonspecific manifestation of the disease can mimic other infectious diseases such as malaria, typhoid fever, and meningitis. Confirmation is done by numerous diagnostic methods, including RT-PCR. Supportive care (rehydration with oral or intravenous fluids) and treatment of specific symptoms improve survival.
There are no licensed vaccines or treatments for the prevention and treatment of Sudan virus disease.
Uganda has reported four outbreaks of SVD, in 2000, 2011 and 2012 (two outbreaks). Uganda also reported an outbreak of Bundibugyo virus disease in 2007 and an outbreak of Ebola virus disease in 2019.
Uganda has experience in responding to Ebola virus disease and Sudanese virus disease outbreaks, and the necessary actions have been quickly initiated. The current outbreak is the first of Ebola caused by the Sudan virus in Uganda since 2012.
In the absence of licensed vaccines and therapeutics for the prevention and treatment of Sudan virus disease, the risk of a potentially serious impact on public health is high. Community deaths and patient care in private facilities and hospitals and other community health services with limited protection and infection prevention and control measures carry a high risk of many chains of transmission. Investigations are underway to determine the extent of the outbreak and the possibility of it spreading to other districts. Importation of cases to neighboring countries cannot be ruled out at this stage.
Based on currently available information, the overall risk has been assessed as high at the national level taking into account: (i) the confirmed Sudanese virus and the lack of a licensed vaccine (ii) the possibility that the event started three weeks before identification of the index case and various chains of transmission have not been traced; (iii) patients presenting to multiple facilities with suboptimal infection prevention and control (IPC) practices, including inappropriate use of personal protective equipment (PPE); patients died and were traditionally buried with great reunion ceremonies; (iv) although the country has developed increased capacity to respond to Ebola outbreaks in recent years, and has local capacity that can be easily mobilized and organized with available resources to mount a robust response, the system could be overwhelmed if the number of cases increases and the outbreak spreads to other sub-counties, districts and regions, as the country responds to multiple emergencies simultaneously, such as anthrax, COVID-19, Rift Valley fever and yellow fever, as well as to floods and the prevailing food insecurity.
Additionally, the outbreak was detected among people living around an active local gold mine. Mobility among traders of this product is likely to be high, and the declaration of the outbreak may cause some miners who are already incubating the disease to flee.
The currently affected Mubende district has no international borders. However, the risk of international spread cannot be ruled out due to active cross-border population movement. In addition, investigations are underway to establish chains of transmission and the extent of the outbreak has not yet been determined.
Regionally and globally, the overall risk has been assessed as low.
Effective outbreak control relies on the application of a package of interventions, including case management, surveillance and contact tracing, optimal laboratory service, implementation of infection prevention and control measures in settings health care and community services, safe and dignified burials, and community participation and social mobilization. Community involvement is essential to successfully control outbreaks. Raising awareness about the risk factors for Ebola infection and the protective measures people can take is an effective way to reduce human transmission.
Early initiation of supportive treatment has been shown to significantly reduce deaths from Ebola. Surveillance and other response activities need to be strengthened to contain the possibility of exponential spread.
Based on available evidence, the ERVEBO vaccine, used in recent responses to Ebola virus disease outbreaks, will not provide cross-protection against Sudan virus disease.
The Johnson & Johnson (Janssen) vaccine called Zabdeno/Mvabea against Ebola has only been approved by the European Medicines Agency (EMA) against Ebola virus disease and has not been tested against Sudan virus disease . This vaccine is given on a two-dose schedule and requires 56 days between doses. The first dose provides protection against Zaire ebolavirus and the second dose was designed to provide protection against other species of the virus, including Sudan. However, this multiantigen protection has not been demonstrated with clinical data. Even if the vaccine were to be tested and found to be effective against Sudan ebolavirus, it would only provide protection a few days after the second dose was given. This means that the vaccine is not appropriate for an outbreak response.
WHO advises against any travel and/or trade restrictions to Uganda based on available information for the current outbreak.
Source: news.google.com